The musculoskeletal system is the most important part of our body. Often, back pain causes the need to see a doctor.
The cause of frequent back pain, stiffness of movement and muscle spasm is osteochondrosis of the back - a disease of bone and cartilage tissue, as well as the musculoskeletal system, caused by various factors affecting the body.

Back osteochondrosis is a problem faced by many people.
Etiology and pathogenesis of osteochondrosis
Dorsal osteochondrosis manifests itself gradually, affecting in latent form all new zones of the spinal space. Initially, changes occur in the structure of the spinal cartilage discs: they lose elasticity, the space between the vertebrae is reduced, and the nerve endings of the spinal cord are violated.
The patient began to experience back pain. Subsequently, the changes overcome the structural elements of the smaller vertebrae, the growth of degenerative bone tissue develops, which impedes the movement of the spine, healthy cartilage cells are destroyed, the disease affects the bones and ligaments. As a side effect, vertebral deformities cause increased load on organs and arteries. This is due to the specificity of the blood supply - the displacement of spinal segments causes compression of the vertebral arteries and, ultimately, is the cause of serious disruption of blood flow in the central nervous system.

The main problems that cause violations of the formation of the spine and the process of osteochondrosis are lack of nutrition and decreased blood supply to the tissues of bone structure. The causes of development are many external factors, internal influences and processes of one’s behavior.
Endogenous (internal) causes include:
- hereditary factors;
- violation of the metabolism of trace elements (phosphorus and calcium);
- cartilage tissue characteristics;
- age -related changes in the body;
- overweight;
- orthopedic diseases.

As a result of exogenous (external) causes and lifestyle, osteochondrosis develops as a result of:
- low level of physical development of the back muscles;
- spinal cord injuries;
- incorrect posture, scoliosis;
- improper or uncomfortable systematic posture;
- unbalanced diet, eating fatty snacks;
- uneven physical exercise, back load;
- bad habits;
- constant pressure.
The latent form of osteochondrosis can be manifested by sharp weight lifting, jumping, falling, which will provoke microtrauma of the spinal disc and violation of nerve roots.
It is then that the patient can feel a sharp shooting pain. In the future, recurrent pain syndromes with varying intensity. Affected nerve stem cells indicate the need for immediate medical intervention.
Disease classification, main rank
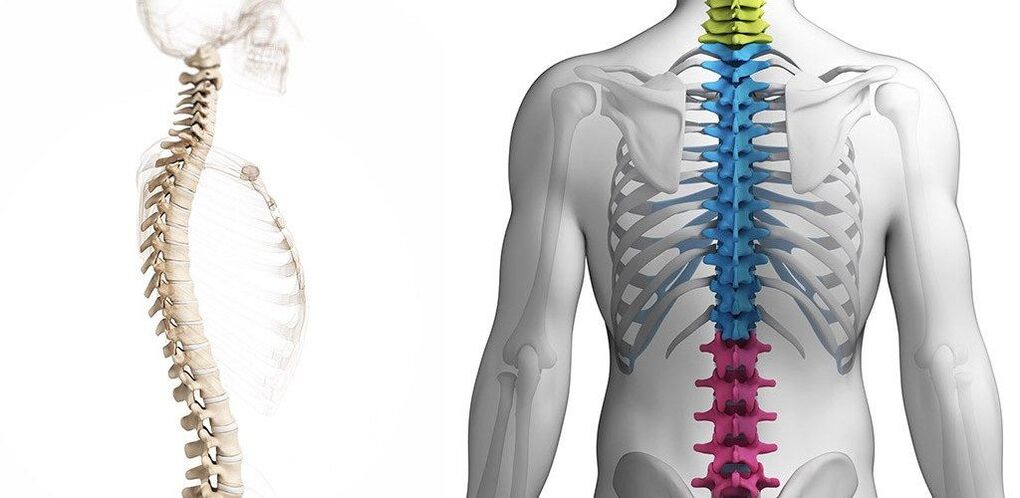
In medicine, osteochondrosis is classified depending on the area of the spine affected:
- cervix;
- dada;
- lumbar and sacral regions.

Dorsal osteochondrosis is classified depending on the area affected.
The main stages of development of this disease:
- The beginning of the development of osteochondrosis - microcracks form in the annulus of the fibrosus, moisture is lost from the bones and cartilage tissue. This stage is manifested by discomfort in one of the zones of the spine after doing physical exercise or an uncomfortable body position.
- The first painful attacks make themselves felt. In the second stage, the disc undergoes protrusion, the intervertebral space of the disc is reduced and the fibrous capsule collapses, the nerve root is pinched. Pain marks the process of metabolic disorders in cartilage tissue and its destruction. Ignoring the second stage of osteochondrosis becomes an impetus in cartilage inflammation and, as a consequence, a violation of nerve fibers, blood vessels and lymph.
- In the third stage of the disease, the affected vertebrae are deformed, the cartilage tissue is removed. With proper active treatment, it is possible to stop cartilage cell destruction and further curvature of the spine. But in the future, supportive therapy and treatment will be the patient’s companion to normal physical activity.
- Launching osteochondrosis, which has entered the last fourth stage of development, is often the cause of disability. All destructive processes are irreversible: significant displacement of vertebral structures, compaction of cartilage tissue, pathological growth of bone tissue. The patient experiences pain, sometimes unbearable, with every movement.
Symptoms
The signs of the development of articular osteochondrosis are easily confused with other diseases that are similar in symptomatology. Also, manifestation symptoms for sectors separate from the vertebral structure have special features.

The main symptoms of osteochondrosis include:
- stiffness while moving, crackling, cracking, or heavy;
- pain in the area of localization of inflammation (cervical, thoracic or lumbar) with varying intensity and character;
- limb numbness;
- muscle weakness, impaired performance;
- attacks of pain, radiating along nerve channels to related parts of the body (shoulders, shoulder blades, legs).
Cervical osteochondrosis
Osteochondrosis of the cervical sector is expressed in the following diseases:
- pain in the neck or back of the head;
- dizziness;
- tinnitus, hearing and vision impairment;
- neck fatigue after sleep or maintaining the same posture for a long time;
- a painful sensation when turning the head.

With cervical osteochondrosis, dizziness and painful sensations may occur while turning the head. The appearance of the first painful sensation is observed in the back of the head and is similar to the head. Inflamed cartilage pressure on nerve fibers, provokes vasospasm.
Osteochondrosis of the chest
The development of thoracic osteochondrosis can be long -term closed to cardiovascular disease. Characteristic symptoms:
- violation of the sensation of touch and numbness of the limbs;
- tingling in the intercostal space;
- pain in the heart area, heart rhythm disturbances;
- restriction of respiratory function, heaviness in the sternum;
- gastrointestinal tract disorders (pancreatitis, bloating);
- radiating pain to the scapular area.
Lumbar osteochondrosis
Progressive lumbar osteochondrosis in its advanced form can lead to disability. The inflamed area of the spine stops the provision of trace elements needed to the lower part of the foot for full functioning of the joints and muscles. Pinching nerve stem cells cause unbearable back pain and the use of drug therapy.
The main symptoms of lumbar osteochondrosis include:
- numbness of the lower limbs;
- muscle pain, weakness;
- shivering;
- muscle cramp;
- reproductive system dysfunction;
- the pain may be sharp or painful in the lumbar region, radiating to the legs.

Diagnostics
On average, there are 20 people with osteochondrosis diagnosed per 1000 population. Diseases such as osteochondrosis are difficult to diagnose at an early stage. The symptomatology is quite hidden and clearly visible only at level 2-3, when it comes time for serious drug treatment.
If there is a suspicion about the development of osteochondrosis, first of all, it is necessary to consult a specialist and conduct a comprehensive examination for a differential diagnosis and clarification of the diagnosis.
Doctors use three standard diagnostic types:
- Neurology.
- Instrumental.
- Laboratory.
The primary neurological examination of the patient is performed by a neurologist, determining the category of nerve structures affected by the disease. Also, to exclude diseases with different properties with similar symptoms, patients can be sent for X-rays, ultrasound, MRI and ECG.
Laboratory (Analysis)
Laboratory diagnostics are advice - added value. Blood tests showed an increase in erythrocyte sedimentation rate and a decrease in calcium levels. This means the course of pathological processes in the body, but does not indicate the specifics of its development. Therefore, this method is included in the thorough examination of the patient and the results are analyzed based on other medical data.

Instrumental
Diagnostics using professional equipment gives the most accurate results on different diseases. The main research tools are:
- X -rays - reveal anatomical changes in bone tissue, cartilage, nerves.
- MRI - Magnetic Resonance Imaging. Allows you to imagine the processes that take place in bones and soft tissues, blood vessels and nerve fibers.
- CT (computed tomography) - similar to MRI, but produces radiation.
- Electromyography - can describe neurological symptoms.

Traditional treatment
Treatment regimens for osteochondrosis are traditional. Its components are drug therapy with multiple directions: NSAIDs, chondroprotectors, analgesics, hormonal agents and supportive vitamin complexes. In addition to the load on the body with drugs in the fight against osteochondrosis, physiotherapy, manual therapy, reflexology, surgery, massage and preventive measures are used.

Drug therapy
It is not possible to stop back pain due to osteochondrosis forever, but medical therapy with medications will provide relaxation in the lower back. Strong anesthetic and anti-inflammatory drugs (NSAIDs) will provide analgesic effects and initiate the process of fighting inflammation in the spinal area. Indispensable drugs for the treatment of back osteochondrosis:
- Chondroprotectors are active ingredients that restore cartilage tissue elasticity and vertebral mobility.
- Muscle relaxation - soothing muscle structure spasms.
- Vascular - improves blood circulation and metabolic processes.
- Vitamin and antioxidant complex.
Only when using a properly selected therapeutic complex, positive dynamics can be achieved and the result maintained for a long time.
In the treatment of posterior osteochondrosis, various forms of medication are used:
- External remedies: ointments, creams, gels.
- Preparations for internal use: capsules, tablets.
- Medication injections.
Surgical intervention
Unfortunately, there are cases of osteochondrosis, when the treatment time is delayed and medications do not give the expected results, and the disease persists. So the only solution is surgery. The main reasons for the operation are:
- Removal of an intervertebral hernia that compresses the spinal cord.
- Reduction of intervertebral fissures to 1/3 of the original size.

Referral for surgical intervention can be prescribed by a physician based on a complete diagnostic picture of the patient and the availability of direct indications for the elimination of pathological defects. In spinal surgery, the main place is taken by the method of discectomy - surgery to remove the disc with deformation. The instrument can be a microdiscectomy, a B-Twin system, or core laser evaporation. Recovery after spinal surgery lasted for six months.
Gymnastics
An excellent supportive therapy for the treatment of osteochondrosis is gymnastics or exercise therapy. Regular exercise will help:
- Strengthen the muscular corset - this is needed for a flat load on the spine.
- Provides circulatory stimulation to meet bone and muscle tissue.
- Develop proper body posture.

It is important to remember that training must be tailored to the diagnosis and adhere to the following principles:
- Frequency of execution.
- Smooth movement, lack of jerks.
- If a painful sensation arises, you need to reduce the load or stop training.
- Monitor your well -being.
Physiotherapy
Physiotherapy is indicated for patients with posterior osteochondrosis to relieve inflammation and is performed in places where the disease is concentrated. The course of treatment contributes to:
- Increases endurance.
- Restoration of metabolism in the affected sector.
- Relieves pain and swelling.
- Improves blood vessel circulation.

To choose a physiotherapeutic method to treat osteochondrosis, you need to clearly define the desired outcome. Mainly used:
- Laser therapy.
- Ultrasonic exposure.
- Electrical stimulation.
- Magnetotherapy.
Diet
There is no single dietary option for patients with osteochondrosis. However, doctors make a unanimous agreement that it is not recommended to use products from the following categories with this diagnosis:
- Fat soup soup.
- Pork and other fatty meats.
- Animal fats of birds (geese, ducks).
- Coffee, caffeinated beverages.

In addition, alcohol and sweets are limited on the menu.
As an example of a diet, you can take diet number 15. It includes all macro nutrients, minerals, vitamins and carbohydrates. The correct menu energy value must be at the level of 2600-2700 kcal, which is equivalent to 85-90g of protein, 350-400g of carbohydrates and 90-95g of fat.
Therefore, the appropriate menu for patients with osteochondrosis is a combination of balanced non -nutrient foods rich in vitamins and minerals. The food is divided into small portions 6 times.
Traditional treatment
Folk remedies are often used at home to relieve inflammation, relieve pain and muscle cramps, and generally strengthen the body. There are many recipes for decoction and incorporation of traditional medicine, which are used in three main ways:
- rubbing;
- compress;
- herbal bath.

Daily use allows you to get rid of discomfort in 10-14 days. Conventionally, folk remedies can be divided into systemic and local effects on the body.
System Tools
To affect the whole body and spine, you can use natural systemic preparations in the form of a decoction.
An example of a positive effect is the action of a decoction of yarrow, which relieves pain, fights inflammation and soothes.
Local funds
Local remedies for folk formulations include ointments, injections for compresses and rubs. These funds must be mixed according to the recipe and applied to the inflamed area, but only if there is no allergy to the components and damage to the skin. Among the popular compositions, special attention is paid to honey compresses, ginger ointment on the pharmacy color of calendula, a mixture of banana and sage herbs, rubbed with carrots with vodka.

To choose an effective method and recipe, you need to consult your doctor, because the method of treatment at home is only part of the general therapy and has only additional effects.
Prophylaxis
Therapeutic therapy for back disease cannot achieve long -term success without preventive measures. Even the most effective and expensive medications do not guarantee the return of symptoms as a result of a return to the body’s daily stress. Therefore, positive effects must be consolidated and maintained using a few simple rules:
- Do not lift more than 10 kg.
- Monitor load distribution on the back muscles.
- Pay attention to rationality and balance in nutrition.
- Take restorative vitamins and active supplements (mucopolysaccharides).
- Develop a regime to change rest and work.
- Maintain physical activity.
Remember that this category of disease is latent. Therefore, when a diagnosis is made, posterior osteochondrosis should not be allowed to run, even if there are no obvious symptoms. Following all doctor’s recommendations and treatment at home allows you to return to a normal work sequence after treatment more quickly, but constant monitoring is needed to prevent deterioration.


























